Tibialis Posterior Tendinopathy
(tendon pain down the inner ankle with or without flat foot )
Information and exercise leaflet for patients and carers
What is Tibialis Posterior Tendinopathy?
Tendon pain down the inner side of the ankle and foot is called Tibialis Posterior Tendinopathy. The Tibialis Posterior tendon is a cord-like structure that passes from your inner calf muscle, down underneath the instep/arch of the foot. When the tendon pulls, it lifts the instep upwards increasing the arch, makes us go up on our tiptoes and helps to push us forwards when walking, running and jumping. It also helps us lower onto the foot when coming down steps. The pain, and sometimes swelling and warmth, is usually felt at the inner side of the ankle and foot.
Tendinopathy is a condition that involves pain and reduced strength in a tendon. This often occurs following a change in activity levels. It may involve you doing more activity than previously, however it can also be a result of doing less than you would normally for example, after a period of illness or extended rest.
The result is that the reduced strength in your tendon means the activities you do now are too much for you to tolerate, and can cause pain.

Common features
Most people will experience pain after rest and first thing in the morning, worse on the inner side of the ankle and foot, as well as after lots of activity like walking.
People will often feel that they are walking very ‘heavily’ and like they have no spring in their step. People might notice that they have developed ‘fallen arches’ or very flat feet.
Full recovery can take between 4 and 12 months.
Should I be resting or moving?
You are safe and generally better off if you move. There is no evidence to suggest your tendon is at greater risk of damage, however it is often helpful to take the strain off the tendon with an appropriate insole that can be prescribed by a podiatrist.
If you keep still and significantly reduce your activity levels, your tendon strength will reduce further and this may lead to further pain and reduced function.
Activity Diary and Modifications
It is sometimes useful to make a note of the daily activities that can potentially aggravate your symptoms. Below are some of the main aggravators and some modifications you can make to help reduce the painful reaction.
Aggravator |
Modification |
|
Walking barefoot |
Ensure you wear supportive footwear, even indoors (rather than slippers). Often a heel raise/support can be effective in improving symptoms. |
|
Sitting down or resting for too long |
Try to avoid prolonged rest. Break up periods of sitting by getting up and moving every 20-30 mins. |
|
Exercising through pain and for prolonged periods. |
Use the reaction rules guide below to ensure that you do not cause a painful reaction. |
How do I know if my activities are causing a painful reaction?
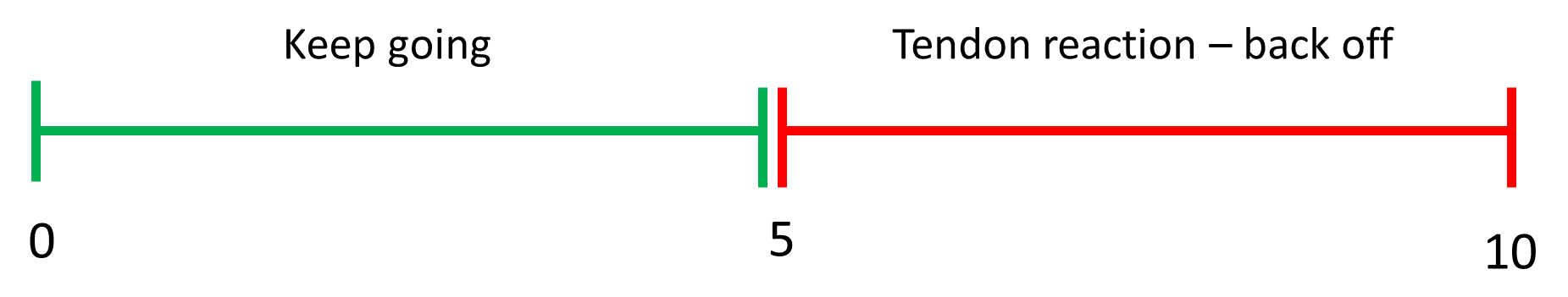
It is common to get a painful reaction if too much load is put through the tendon. If this pain is more than 5/10 (with 10 being the worst pain imaginable) and lasts for more than 24 hours, check what you have been doing and ease back, not necessarily stop/avoid in future.
Once this has settled you can start to gradually introduce your activities and exercises again. If you have a mild aggravation (pain is less than 5/10) and this settles within 24 hours then keep going with your exercises and gradually return to full activities (see below).
Pain relief and injections
Painkillers can help you keep moving. However, it is important to discuss this with your GP, especially if you are taking any other medication.
Injections are not recommended for this problem.
What about sports/work?
You should use the previously mentioned reaction rules to highlight whether a return to sport or work is advisable at this stage.
Do I need any tests?
Tibialis Posterior Tendinopathy is diagnosed clinically. Scans and other investigations are often not recommended as they are not required. An X-Ray can be used to rule out any significant Osteoarthritis in the area.
What are the aims of management?
Management of this condition always requires some physiotherapy. The aims of physiotherapy are to improve muscle strength, load tolerance and pain in your tendon and improve function through your foot and ankle. This should allow you to return to your previous activities.
Management of this condition sometimes requires a prescribed insole (orthotic device) that supports the arch/instep and reduces load/strain on the tendon. This can allow activities like walking to be less painful and more efficient as well as allowing the painful tendon reaction to settle.
General measures to help
If you are overweight, try to lose some weight as the extra burden placed on your tendon can make symptoms worse. Even a modest weight loss can make quite a difference.
Poor diet, high cholesterol and diabetes can also be linked to developing a tendinopathy.
Warning Signs
If you develop new or worsening symptoms, if you are unwell with the pain, or under the age of 16 years, seek medical advice.
The following symptoms are very rare, but if you suddenly develop any of them, you should seek urgent medical attention at your local Urgent Care Centre.
- Sudden onset of Achilles pain, with a “pop” or snapping sound/sensation.
- Inability to weight-bear through the foot/ankle.
- New significant injury to the leg/foot/ankle.
- Constant night pain in the foot/ankle (that prevents rest/sleep).
- Significant swelling, colour change or temperature change in the foot/ankle or extending up the leg.
- Lumps in the foot/ankle.
- Signs of infection i.e. night sweats that are out of the ordinary, high temperature and feeling unwell.
- Unexplained weight loss
If your symptoms fail to improve within 6-8 weeks with this regime you should contact your doctor for a physiotherapy referral.
If your symptoms are improving (even slowly), continue for up to 3 months.
Exercises for Tibialis Posterior Tendinoapthy
The exercises below are in order of difficulty. Start with the first and if this does not increase your symptoms progress to the next one.
Use the reaction rules to guide your exercise intensity. If pain is stopping you engaging in rehab, you should speak to your GP about pain relief promptly.
Flare-ups may happen - if it doesn’t settle in a couple of weeks, then seek further advice.

Heel Raises Sitting
Sit upright on a chair, with your feet flat on the floor. Slowly raise your legs up onto your toes. Hold, and gradually control the movement back down to the starting position. This is a useful calf pump exercise to improve circulation to your lower legs, as well as improving mobility of the ankle joints.
Perform 10 times Repeat 5 times 3 times daily

Towel Pick-Up
Sitting on a chair, cross your feet keeping your heels on the floor. Push the outside of your feet against each other. This is a strengthening exercise for your ankles.
Perform for 30 seconds Repeat 5 times 3 times daily

Self-Resisted Eversion
Sitting on a chair, cross your feet keeping your heels on the floor. Push the outside of your feet against each other. This is a strengthening exercise for your ankles.
Hold for 30 seconds Repeat 5 times 3 times daily

Calf raises
Stand upright and hold onto a wall/table for balance if required. Slowly raise up onto your toes, and control the movement back down. This exercise will strengthen the calf muscles and ankle joints. Repeat for the repetitions suggested, or until muscle tiredness or discomfort
Perform 10 times Repeat 5 times 3 times daily
Once you are able to perform 30 reps in one go, progress to trying to do it on the affected leg only, holding on to something for balance
What actions can I take to improve my health?
Evidence tells us that making healthy lifestyle choices can have a big impact on influencing problems with your muscles and bones and can play a major role in your overall health. Some of the most effective areas to address are below: (click on the links)
Maintaining a healthy weight: www.nhs.uk/live-well/healthy-weight/
Increasing levels of physical activity: www.nhs.uk/live-well/exercise/
Avoiding poor sleep patterns: www.nhs.uk/live-well/sleep-and- tiredness/how-to-get-to-sleep/
Reducing alcohol consumption: www.nhs.uk/live-well/alcohol- support/calculating-alcohol-units/
Stopping smoking: www.nhs.uk/live-well/quit-smoking/
Maintaining a healthy mind: www.nhs.uk/conditions/stress-anxiety- depression/
The good news is that you are able to influence lots of these by modifying your lifestyle. Therefore it is important that you consider addressing these areas alongside your current treatment.
You may wish to discuss any of these factors with your treating clinician who will be able to work with you and guide your long term management and support you to improve your wellbeing.
There will be information about the local services that exist within the waiting areas of the physiotherapy department and your treating clinician will be able to help signpost you to appropriate services.
The websites listed below give more information on local services available:
• Blackburn and Darwen - https://refreshbwd.com/
• East Lancashire - http://www.upandactive.co.uk/
Public Health England https://www.gov.uk/government/organisations/public-health- england
Review Date: January 2024