Information and exercise leaflet for
patients and carers
What is Carpal Tunnel Syndrome (CTS)?
Carpal Tunnel is a condition that is caused by compression of the median nerve as it passes through the carpal tunnel at the wrist. The carpal tunnel is formed by the wrist bones on one side and a thick ligament on the other.
The median nerve is responsible for supplying the sensation to the thumb, index, middle and a portion of the ring fingers. These are the most affected fingers, although sometimes the whole hand and on occasion the forearm can also be affected. CTS affects more women than men and is most common in those aged 40-65 years.
What are the symptoms of carpal tunnel syndrome?
CTS can have one or both hands and cause a variety of symptoms, including tingling / numbness and sometimes pain into the area which the median nerve supplies. You may also experience a feeling of swelling or clumsiness to the hand. Symptoms are often worse at night, feeling like you need to shake the hand or hang the hand, out the bed. They may also occur through the day, particularly with activities such as writing, typing, DIY and housework.
It can affect either just one or both hands.
In the later stages of CTS, you may notice weakness to the fingers and thumb, gripping objects, or problems with fine finger movements such as fastening buttons. In these cases, you may notice wasting on the muscles around the thumb.
What causes Carpal Tunnel Syndrome?
Any condition that reduces the amount of space within the carpal tunnel can cause CTS. The median nerve is very sensitive to pressure. The following is a list of things that can increase your risk of developing CTS (but not limited to):
- Metabolic conditions i.e., Diabetes, Thyroid gland imbalance
- a wrist fracture
- Inflammation, and conditions related i.e., rheumatoid arthritis
- Fluid retention (for this reason CTS can occur in pregnancy)
- Hormonal changes associated with the menopause
- Your genes
- Obesity
- Occupation or sports that places heavy demand on your wrist - using vibration tools / repetitive gripping
- Occasionally some medications may cause it.
What treatments are there for carpal tunnel syndrome?
Not all cases will cause long term symptoms and for some people you may find it improves without any medical treatment. Likewise, if there is a particular cause for your problem such as under active thyroid gland or arthritis, treating the cause, may improve the CTS symptoms.
However, there are different treatments that can help reduce or prevent the symptoms of CTS, which we will discuss in more detail.
Splints
Wearing a splint whilst you are sleeping may reduce the severity of your symptoms, by allowing inflamed areas to rest. Also, the positioning of the wrist is important to reduce the pressure within the carpal tunnel. The carpal tunnel is under its least amount of pressure when the wrist is straight.
It can take several weeks before you start to notice an improvement in your symptoms, therefore if tolerated it is sensible to trial splints for at least 8-12 weeks. Splints are to be worn at night. They are to keep the wrist in a straightened position. The splint straps should be firm but not too tight, so that circulation is not affected. Please seek advice if you feel any skin irritation, colour changes to the skin, increased swelling, rubbing, increased pain or pins and needles in the hand /wrist /forearm.
Splints Hygiene – splints can be washed in cold soapy water, remove the metal bar before doing so. Also splint liners can be considered for comfort and to enable you to wash more regularly.
Altering your activities
Some activities may increase the severity of your symptoms and altering these, where you are able, may reduce your symptoms:
- Avoiding extreme positions of the wrist; this may involve reviewing your workplace set up and consider use of aids.
- Modify your environment; for example, using wider grip tools/ cutlery, or handles for equipment.
- Posture: The nerves begin at the neck and travel the length of the arm; therefore your overall spinal and upper limb posture should be considered. (See figures below as good examples)
- Reduce the duration or frequency of aggravating activities, taking regular breaks, altering grip.


Injections
A steroid injection may be offered following a thorough assessment by your clinician. This is where a small amount of steroid is injected into the carpal tunnel, to aiming to reduce any inflammation. This may be helpful; however, responses cannot be guaranteed, and symptoms may return.
Exercises
Median nerve glides
These exercises aim to gently glide the nerve and tendons through the carpal tunnel.

Stand or sit with good posture, and take your affected arm out to the side at 90 degrees with your elbow bent.
Bend the wrist backwards so the palm is facing up. This is the start position.
Bend your neck towards the affected side, and slightly straighten your elbow, then bend the neck to the opposite side as you bend your elbow.
Repeat 5 times x 5 times per day
Wrist
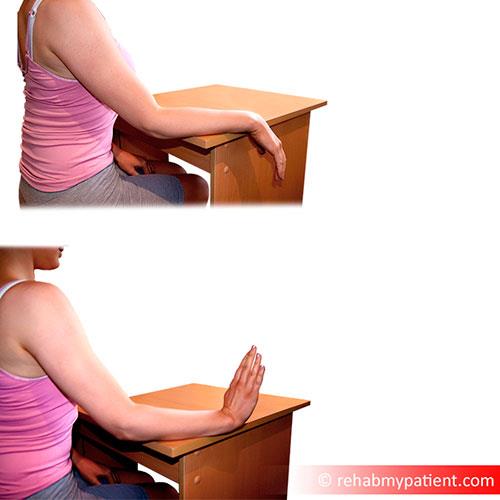
Whilst keeping your elbow still, bend your wrist down and back keeping your fingers relaxed.
Carry out x 10 repetitions of each exercise x 5 sessions a day.
Tendon Glides
Start with the fingers and wrist straight every time. Do each exercise 5-10 times per session with a 1 second hold and carry out 5 times a day.



Hook Fist
Partial Fist
Full Fist
Please note:
If you feel an increase in pain or symptoms which does not reduce after 2 hours of doing the exercises please talk with your physiotherapist, please also ask if you have any further questions or concerns.
What actions can I take to improve my health?
Evidence tells us that making healthy lifestyle choices can have a big impact on influencing problems with your muscles and bones and can play a major role in your overall health. Some of the most effective areas to address are below: (click on the links)
Maintaining a healthy weight - www.nhs.uk/live-well/healthy-weight/
Increasing levels of physical activity - http://www.nhs.uk/live-well/exercise/
Avoiding poor sleep patterns - www.nhs.uk/live-well/sleep-and-tiredness/how-to-get-to-sleep/
Reducing alcohol consumption - https://www.nhs.uk/live-well/alcohol-support/calculating-alcohol-units/
Stopping smoking - http://www.nhs.uk/live-well/quit-smoking/
Maintaining a healthy mind - http://www.nhs.uk/conditions/stress-anxiety-depression/
The good news is that you are able to influence lots of these by modifying your lifestyle. Therefore, it is important that you consider addressing these areas alongside your current treatment.
You may wish to discuss any of these factors with your treating clinician who will be able to work with you and guide your long-term management and support you to improve your wellbeing.
There will be information about the local services that exist within the waiting areas of the physiotherapy department and your treating clinician will be able to help signpost you to appropriate services.
The websites below give more information on local services available:
- Blackburn and Darwen: https://refreshbwd.com/
- East Lancashire: http://www.upandactive.co.uk/
- Public Health England: https://www.gov.uk/government/organisations/public-health-england
Applications (Apps)
The ORCHA website will recommend useful and rated apps to support your wellbeing. https://www.orcha.co.uk/
Aims of Physiotherapy
Physiotherapy may form one part of your management, helping you identify the main contributory factors whilst working together to plan your rehabilitation.
Your physiotherapist may spend time talking with you about your hand pain, providing advice, reassurance and helping discuss any concerns you may have.
A physiotherapist can provide and help oversee a personalised exercise programme focused on what you want and need your body to achieve.
Warning Signs
If you have severe pain which is getting worse over several weeks, if you are unwell, or under the age of 16 years, you should consult your doctor. The following symptoms are very rare, but if you suddenly develop any of them, you should consult your doctor straightaway.
- Significant swelling to the arm
- Feeling generally unwell
- Sign of infection i.e. does your joint feel hot and swollen to touch compared to the other side, night sweats that are out of the ordinary, high temperature and feeling unwell.
- Constant night pain (unable to rest/sleep)
- Unexplained weight loss
- Loss of control of hand movements or strength or grip (dropping objects)
If your symptoms fail to improve within 6 weeks with this regime you should contact your doctor for a physiotherapy referral.
You can download a printable version of this information here.
Please note this is a PDF and does not meet accessibility needs.


