(with or without leg pain)
Information and Exercise Leaflet
for Patients and Carers
Back pain is very common at all ages of adulthood. 8 out of 10 people will have back pain at some point in their lives and 90% of these cases resolve without specialist input.
- In most cases it is not due to a serious disease.
- Back pain can be associated with a range of sensations. This may present as anything from stiffness, tight/achy muscles to sharp localised/stabbing pains. Occasionally the nerves can become irritated and cause pain, pins and needles and sometimes changes to your feeling in that area. These symptoms are not frequently associated with serious disease or injury.
- Investigations such as X-ray and MRI are rarely beneficial for the diagnosis and physiotherapy management of back pain.
- The spine is strong and resilient and in most cases, back pain improves of its own accord within 6-8 weeks with 8 out of 10 people reporting an improvement in their symptoms after just 4 weeks.
- Keeping active is crucial to assist with recovery of back pain.
- Why does my back hurt?
- There are many factors that can contribute to developing back pain:
- Physical effort that exceeds your capability. All joints and soft tissues in the body have a certain capability for activity that they can tolerate. This can depend on how much activity you normally do and how well your body has adapted to this activity over a period of time. If you do an activity that takes you over this level you can present with a painful reaction.
For example, if you perform an activity such as digging your garden for longer than your joints and tissues can tolerate, you can cause overload and irritation resulting in a painful reaction. This response is protective; the pain is looking after you whilst your tissues settle. It is not an indicator of condition severity and is rarely associated with tissue damage.
- Trauma such as falls, sports injuries and car accidents can expose your body to a rapid change in movement and/or blunt impact. This force can cause injury to the body’s tissues and lead to swelling and inflammation.
- Inactivity and staying in one position for too long. Remember: keeping active is important.
Non-physical factors can also influence your pain such as:
- Emotional stresses for example anxiety, depression; family or occupational issues can make your pain system more sensitive, resulting in you experiencing more pain.
- Lifestyle factors such as disturbed sleep, poor diet, lack of exercise/activity and smoking can also contribute to back pain.
With simple advice provided within this leaflet, your back pain should settle within 6 weeks. It is important that you remain active and continue as normal as much as
possible. However, if your back pain is persistent and severe then you should seek
medical advice for the appropriate treatment.
What about work?
Around 34% of workplace musculoskeletal (MSK) problems (that are related to joints, muscles, ligaments etc.) are of the lower back and your back pain may alter your ability to perform your usual work related responsibilities.
It is important you discuss any concerns or limitations with your employer as remaining in work or returning as soon as you are able is an important contributor to good health.
For free and confidential advice about work, call the Healthy Working Lives Advice Line on 0800 019 2211.
Alternatively, visit the Fit for Work (http://fitforwork.org/) and the HSE website
(https://www.hse.gov.uk/msd/backpain/index.htm) for further resources.
What about sports?
As discussed above, keeping active is crucial to assist recovery of your back pain
however you should pace your return to your sporting activity. You will need to re-start at a lower level than you were used to before and slowly increase this amount. Be prepared, however, for slight discomfort at first and remember to warm up before and cool down following participating in your sport.
What actions can I take to improve my health?
Evidence tells us that making healthy lifestyle choices can have a big impact on influencing problems with your muscles and bones and can play a major role in your overall health. Some of the most effective areas to address are below:
Maintaining a healthy weight - www.nhs.uk/live-well/healthy-weight/
Increasing levels of physical activity - http://www.nhs.uk/live-well/exercise/
Avoiding poor sleep patterns - www.nhs.uk/live-well/sleep-and-tiredness/how-to-get-to-sleep/
Reducing alcohol consumption - https://www.nhs.uk/live-well/alcohol-support/calculating-alcohol-units/
Stopping smoking - http://www.nhs.uk/live-well/quit-smoking/
Maintaining a healthy mind - http://www.nhs.uk/conditions/stress-anxiety-depression/
The good news is that you are able to influence lots of these by modifying your lifestyle. Therefore it is important that you consider addressing these areas alongside your current treatment.
You may wish to discuss any of these factors with your treating clinician who will be able to work with you and guide your long term management and support you to improve your wellbeing.
There will be information about the local services that exist within the waiting areas of the physiotherapy department and your treating clinician will be able to help signpost you to appropriate services.
The websites listed below give more information on local services available:
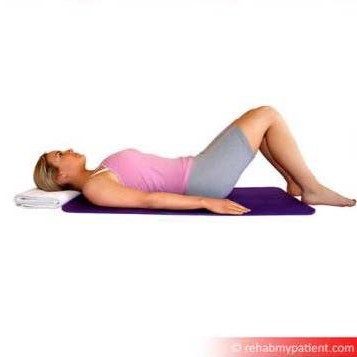
Sleeping Positions
Sleep is really important for healing and reducing pain sensitivity, therefore getting good quality sleep can help you whilst recovering from back pain, you may find these sleeping positions helpful:
If your symptoms are made worse by walking and standing activities; start with the below sleeping positions:
If your symptoms are made worse by sitting and bending activities; start with the below sleeping positions:
If you don’t follow either of the above patterns and your symptoms are worse with any position for a prolonged period of time, try and find which positions benefit you the most from either section and work on those initially.
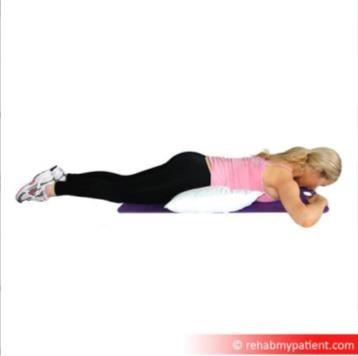
Resting Positions:
Being able to relax your body and mind is an important strategy to aid recovery from back pain; you may find these resting positions helpful:
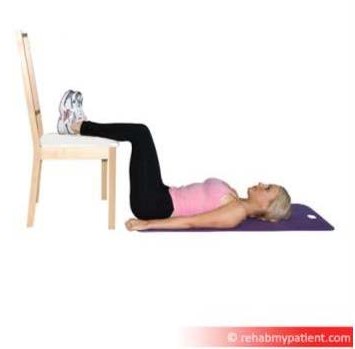
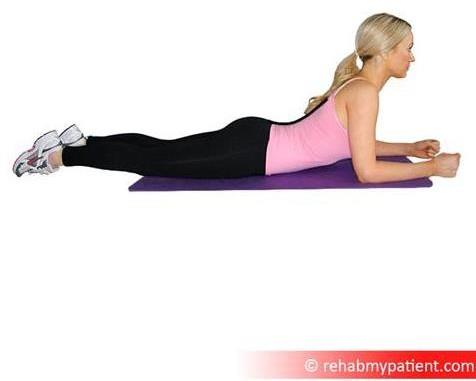
If your symptoms are made worse by walking and standing activities; start with the below resting positions:
If your symptoms are made worse by sitting and bending activities; start with the below resting positions:
If you don’t follow either of the above patterns and your symptoms are worse with any position for a prolonged period of time, try and find which positions benefit you the most from either section and work on those initially.
Applications (Apps)
The ORCHA website will recommend useful and rated apps to support your wellbeing. https://www.orcha.co.uk/
Aims of Physiotherapy:
Physiotherapy may form one part of your management, helping you identify the main contributory factors whilst working together to plan your rehabilitation.
Your physiotherapist may spend time talking with you about your back pain, providing advice, reassurance and helping discuss any concerns you may have.
As mentioned previously, exercise is one of the most effective treatments for back pain.
A physiotherapist can provide and help oversee a personalised exercise programme focused on what you want and need your body to achieve.