The Acute Pain Team (APT) has four nurses, two with prescribing qualifications plus support of a weekly Consultant Anaesthetist. The APT service is provided to the surgical wards Monday - Friday during office hours.

The Acute Pain Team see many patients who are receiving specialised pain relief methods, but not every patient after surgery.
The ward staff are responsible for managing your pain relief, but can ask for advise from the Acute Pain Team if needed.
Pain relief after surgery
- Good pain relief makes it much more comfortable for patients to mobilise soon after their operation
- Our aim is to offer the most safe and effective pain relief available with the minimum side effects
- To regularly assess pain and any side effects
- To provide advice on discharge pain relief
Methods of pain relief

Please inform staff when completing admission paperwork if you already take pain killers regularly as this may influence our approach to your post-operative pain management. Your anaesthetist will discuss post-operative pain relief options with you. It is normal to receive a number of different types of pain relief as each medication works in different parts of the body to reduce pain. This may include medication given by the use of a specialist pump:
- Epidural
- Patient controlled analgesia (PCA)
- Spinal anaesthetic with opiate drug
- Local anaesthetic infusion
- Rectus sheath catheter (RSC)
- Local wound infusion
If one of these specialist pumps is being used it may be for between 3-5 days. After this you will be changed to another form of pain relief. There will be regular monitoring of observations whilst you are receiving pain medication - this ensures that if you are experiencing any side effects they are managed quickly and also makes sure the technique is effective.
Stronger pain killers will be available - these may come in the form of a pain patch or slow release tablets and fast acting morphine liquid.
You will also be given a combination of the drugs below (unless contra-indicated):
- Paracetamol - 4 times in 24 hours
- Ibuprofen - 3 times in 24 hours (approx 3-5 days)
- Gabapentin - 3 times in 24 hours. This drug helps reduce post-operative nerve pain (approx 3-5 days)
- Anti-sickness medication regularly and as required, plus any drugs needed to treat other side effects
Side effects of strong pain medication may include sickness, hallucinations, confusion, itching, numbness or constipation. If you experience any of these, please report them to your named nurse.
How is your pain today?
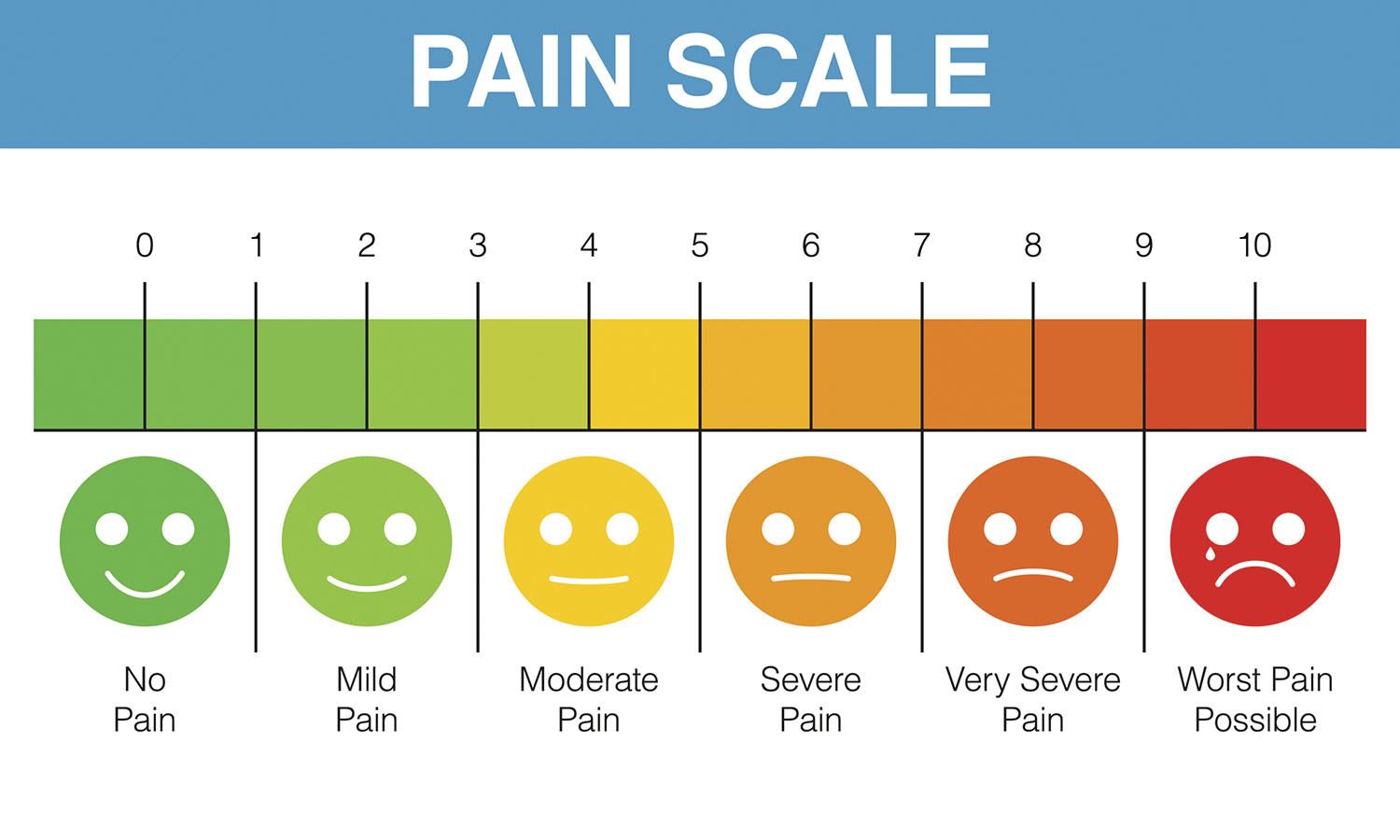
Pain assessment is really important so that staff can understand if your pain is controlled well enough. You will be asked if you have pain on moving, deep breathing and coughing. We ask on a scale of 0 = no pain to 4 = worst pain ever, "how bad is your pain?". It is important that you are honest with us, if you are struggling to let the nurse caring for you know. Experiencing some discomfort is to be expected - but if that pain stops you from moving, deep breathing or coughing then we need to know. You should be prescribed extra breakthrough pain medication that acts quickly and lasts for short periods of time. You can ask the nurse for this at any time of the day or night.
Reducing or stopping your pain relief after surgery
Once you are recovering from your surgery and pain levels are reducing, the doses and types of strong pain relieving medication will be reduced and stopped and this may be before you are discharged home. We expect to use strong morphine type medication for short term only.
If you are taking regular strong pain killers prior to coming into hospital then we will probably reduce you back onto what you usually take as soon as you are able, then your GP can review if these are still needed once you have recovered from the surgery. It may be over time these drugs can be stopped.


